There is (rightly) a lot of buzz these days around the insidious, incremental erosion of a woman’s right to choose whether she will give birth to a child she has conceived, but virtually nobody is talking about the drastic erosion of a woman’s right to choose how she will give birth to her term baby. Who is talking about the shocking erosion of a woman’s right to choose a VBAC (vaginal birth after cesarean)?
I’m inspired to post this by today’s Facebook thread about a woman whose doctor has dropped her from care at 41 weeks because of her desire to have a VBAC. And in portraying the conflicted pressures involved in Leah Marshall’s experience of pursuing a vaginal birth after cesarean (VBAC), author Koa Beck says Marshall sees “her birthing choice as a political one in a health system that, according to her, ‘still treats women as second-class citizens.'”
For one thing, Marshall discovered that she evidently wasn’t entitled to fully-disclosed informed consent. Sure, the common VBAC warning thrums like a drumbeat, incessant and daunting, conjuring an image horrific enough to scare off even the sturdiest among us : risk of uterine rupture. What Marshall was shocked to discover as she did her research was what nobody seems to be talking about, certainly not many doctors: the serious medical risks inherent in having two or more C-sections! (Her delivery nurse mother-in-law told her that “many doctors often don’t feel the need to share this information with their patients given how much smaller modern families are.” Say, what???!!!)
The Repeat C-Section Risk Nobody Talks About
There is a life-threatening condition in which the placenta grows into the uterine wall and sometimes beyond, called placenta accreta. It was once a rare event, affecting 1 in 30,000 pregnant women in the 1950s and 1960s; it now occurs in 1 in 2,500 pregnancies, according to a 2007 report in the Journal of  Obstetrics and Gynecology. In some hospitals, the number is as high as 1 in 522. And doctors say the main reason is the dramatic rise in the number of cesarean sections — about about 38 percent of all pregnancies in New Jersey, the second highest in the nation.
Obstetrics and Gynecology. In some hospitals, the number is as high as 1 in 522. And doctors say the main reason is the dramatic rise in the number of cesarean sections — about about 38 percent of all pregnancies in New Jersey, the second highest in the nation.
“The rule of thumb is if you have one C-section and the placenta sits right on top of the scar, the risk of placenta accreta is 25 percent,” said Dr. Abdulla Al-Khan, director of the Division of Fetal Medicine and Surgery at Hackensack University Medical Center. “If you’ve had two previous C-sections the risk is close to 50 percent and three, it’s 75 percent and four, it’s invariably closer to 100 percent.”
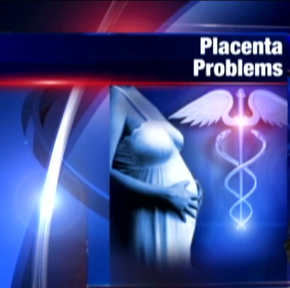 Together with more diabetes and preeclampsia, a higher number of twins and multiples, and advanced maternal age, a rise in the rate of placenta accreta is now suspected to contribute to the rising rate of maternal postpartum mortality — a rate that, by the by, has tripled in California in a decade. This according to Ina May Gaskin; I had the honor of serving as “opening act” for her keynote talk last spring at the “Your Natural Baby Fair” in San Diego, in which she shared this dismal news. We should all be beyond outraged at the statistics.
Together with more diabetes and preeclampsia, a higher number of twins and multiples, and advanced maternal age, a rise in the rate of placenta accreta is now suspected to contribute to the rising rate of maternal postpartum mortality — a rate that, by the by, has tripled in California in a decade. This according to Ina May Gaskin; I had the honor of serving as “opening act” for her keynote talk last spring at the “Your Natural Baby Fair” in San Diego, in which she shared this dismal news. We should all be beyond outraged at the statistics.
Ina May’s VBAC Facts
But back to choice in birth, specifically VBAC. (Coincidentally, the following passage from my book I learned from Ina May as well!)
The VBAC (vaginal birth after cesarean) movement began in 1970 and peaked in1996, when twenty-eight percent of women with prior C-sections gave birth vaginally. The research comparing VBACs with repeat cesarean continued to mount and it all agreed: VBAC trials (meaning attempting a normal vaginal labor, whether or not a cesarean is ultimately performed) were safer for mothers (with transverse lower-uterine incisions) and equally safe for babies; and nearly eighty percent of women who tried VBAC were able to give birth vaginally.
A 1995 position statement — supported by extensive published research evidence — from the American College of Obstetricians and Gynecologists (ACOG) encouraging VBAC and recommending limiting repeat cesareans to those that were medically necessary seemed to ensure that VBAC would remain an option for women. But in a classic retrogressive, maintain-the-status-quo backlash, it only took a few intervening years for medico-legal and economic forces to swoop in and slam the door shut on this choice for women. (Hmmm, that’s a frightening thematic specter…) The evidence didn’t change (and indeed was largely omitted from later ACOG position statements) but the recommendations did, and according to Ina May Gaskin — whose chapter on VBAC is a must-read if you are hoping for one — “Sadly, the newest ACOG recommendations effectively close the door to VBAC to most women. For them it might as well be 1970, when few U.S. physicians conceded that women facing repeat cesareans ought to have a choice in the matter.” (ACOG issued a new position statement in July of 2010 backpedaling on its former restrictive VBAC guidelines, but many birth advocates feel it will do little to change a decade of entrenched physician and hospital policy, or to re-open VBAC access to most women.)
Ironically enough, given this retrogressive effacement of VBAC, the woman who had the first successful cesarean, in 1500 — successful because both mother and baby survived — went on to deliver six more babies vaginally, including twins! Gaskin outlines the impressive VBAC rates at her Farm Midwifery Center, and also mentions the Amish women she knows who’ve had a cesarean for their first baby and gone on to have twelve, thirteen VBACs without complication. She also offers practical advice for those women wanting to pursue VBAC — a richly viable path to take when you understand the territory: 1) choose a caregiver who has a VBAC rate of seventy percent or more (who will be knowledgeable enough to make sure, for example, that your placenta is not overlying your existing uterine scar); 2) do not use synthetic oxytocin, Cytotec, or other prostoglandins to induce or augment labor, since the collected evidence strongly suggest it is these that increase the risk of uterine rupture; 3) keep vaginal exams to a minimum, which is possible with skilled practitioners who can closely estimate dilation by observing your breathing and body language; and 4) avoid an epidural, especially early in a VBAC labor. Last but definitely not least, counsels Gaskin, “spend your pregnancy loving your uterus and your baby. I mean this literally. Positive energy makes a good birth outcome more likely, so go for it.”
Succeeding in Getting a VBAC
“Going for it” includes cultivating what OB/GYN Stuart Fischbein refers to as the “right mental stuff”; if you peruse many of the YouTubes about VBAC — especially HBACs (home birth after cesarean) — you’ll find a common thread: these women found themselves while they were finding their way to a vaginal birth. They journeyed within, dug down, and found their grit. It takes courage to trust your body’s inherent rightness and abilities when culture bombards you with messages to the contrary –like parlors to keep you hairlessly groomed and products to keep you fresh “down there”… and a parade of television and movie scenes continually portraying birth as a horror to simply medicate (or cut) out of your consciousness.
It also take a great deal of grit to defy the medical priesthood in their white robes and stethoscope adornment warning about uterine rupture. Don’t get me wrong. I am not anti-doctor, at all! I still thank God for the doctors who operated on our son (then seven) when his appendix ruptured. That was a true medical emergency. Treating normal, healthy birth like a medical emergency, however, has contributed tremendously to the current soaring cesarean rates, and in turn (though more complicated interrelated causal factors are likely involved) our failing maternal mortality report card.
What’s Really Going On? Follow the Money
The disconnect between the collected evidence and the practices persisting in hospitals across the country is one of the stark realities of an obstetrical industry that is as market-driven as other for-profit industries. The typical cascade of unnecessary hospital birth interventions makes sense, suggests somatic psychotherapist Robert Leverant, “only if you follow the money and not the baby.”
And not the mother. In his report on current proposed legislation that would make midwifery care more widely available, particularly to lower-income families, John Weeks puts his finger like a laser on the dirty little secret spot of greatest push-back to birth reform (which would include Medicaid coverage for midwifery-attended home births), pointing out that it represents disruptive innovation of the highest order for hospitals nationwide, for whom birth is their bread and butter:
“Consider the potentially long-term positive consequences if mothers and families learn that most can have their babies at home, without all that expensive intervention. Might human beings with such an experience of self-care and empowerment in the act of giving birth be more disposed toward achieving self-efficacy in other parts of their care?”
This is why I write in Parenting for Peace that “this is subversive stuff. This book may have innocent little cookies on its cover, but it actually calls for a revolution — an awakening to your own power that comes from within, not from without.”
I will leave you with an astonishing, touching portrayal of self-efficacy… of mother, of baby, of everyone involved here: a gentle, nearly-silent home breech birth. Be sure to watch till at least 5:56, to hear what the new dad says to his baby daughter. This has the power to change hearts. Maybe it can change policy, too.
Sources:
Ina May Gaskin. (2003). Ina May’s Guide to Childbirth. New York: Bantam-Dell.
Images:
Cesarean image by tifhermon under its Creative Commons license.
Aurora’s Birth by Jodie Myers.
by Marcy Axness, PhD, author of Parenting for Peace: Raising the Next Generation of Peacemakers
Tags: birth, C-section, cesarean, choice, informed consent, maternal mortality, placenta accreta, uterine rupture, VBAC